When Medicine is not in Evidence
Photo courtesy Bob Wong
Much has been made in the past two decades or so of the need for “evidence-based medicine.” An article in the British Medical Journal entitled “Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials” made the case that common sense and clinical experience ought not be overruled by overzealous application of the evidence-based paradigm. The authors of the article pointed out that there have been no good-quality clinical trials of parachute use to prevent death and injury due to “gravitational challenge” (i.e. falling out of an airplane). They then asked whether the use of parachutes ought to be tested using the standards of evidence-based research, with a slight catch: “Advocates of evidence based medicine have criticised the adoption of interventions evaluated by using only observational data. We think that everyone might benefit if the most radical protagonists of evidence based medicine organised and participated in a double blind, randomised, placebo controlled, crossover trial of the parachute.” Though the article was tongue-in-cheek, the point it made had serious ramifications: if the evidence-based paradigm was used as a basis to deny payment for treatment by insurance companies, for instance, or to ban untested interventions from use, then the baby would most likely get thrown out with the bathwater (and without a parachute, most likely).
In fact, we would be left with a laughably impoverished medical model, since rigorously studied medicine still makes up a relatively small percentage of what actually is practiced. Surgery, for instance, has typically not been tested in “blind” studies against a placebo, because it is hard to find people willing to get cut up for sham surgery. And though pharmaceuticals must go through a lengthy, expensive review process before approval for particular conditions, many drugs are prescribed for “off-label” uses as well for conditions they were never tested on. Some pharmaceuticals, such as Neurontin (gabapentin), are used more than 80% of the time for conditions that were never tested for the drug (according to Forbes magazine). Though drug manufacturers can get in trouble for actually promoting off-label uses, physicians have wide latitude in prescribing drugs this way. It is a tradition of clinical practice, and ought to remain that way, for doctors to be able to try novel approaches to treating conditions for which there is no other satisfactory treatment or cure. Of course, the risks of the treatment need to be weighed against the potential benefit, and so an honest dialogue between doctor and patient is essential; as patients, we need to know what, if any, evidence there is for any particular treatment, the quality of that evidence, and the known risks involved. Thus, there needs to be a balance between the well-intentioned concept of evidence-based cures and the clinical need for flexibility and innovation.
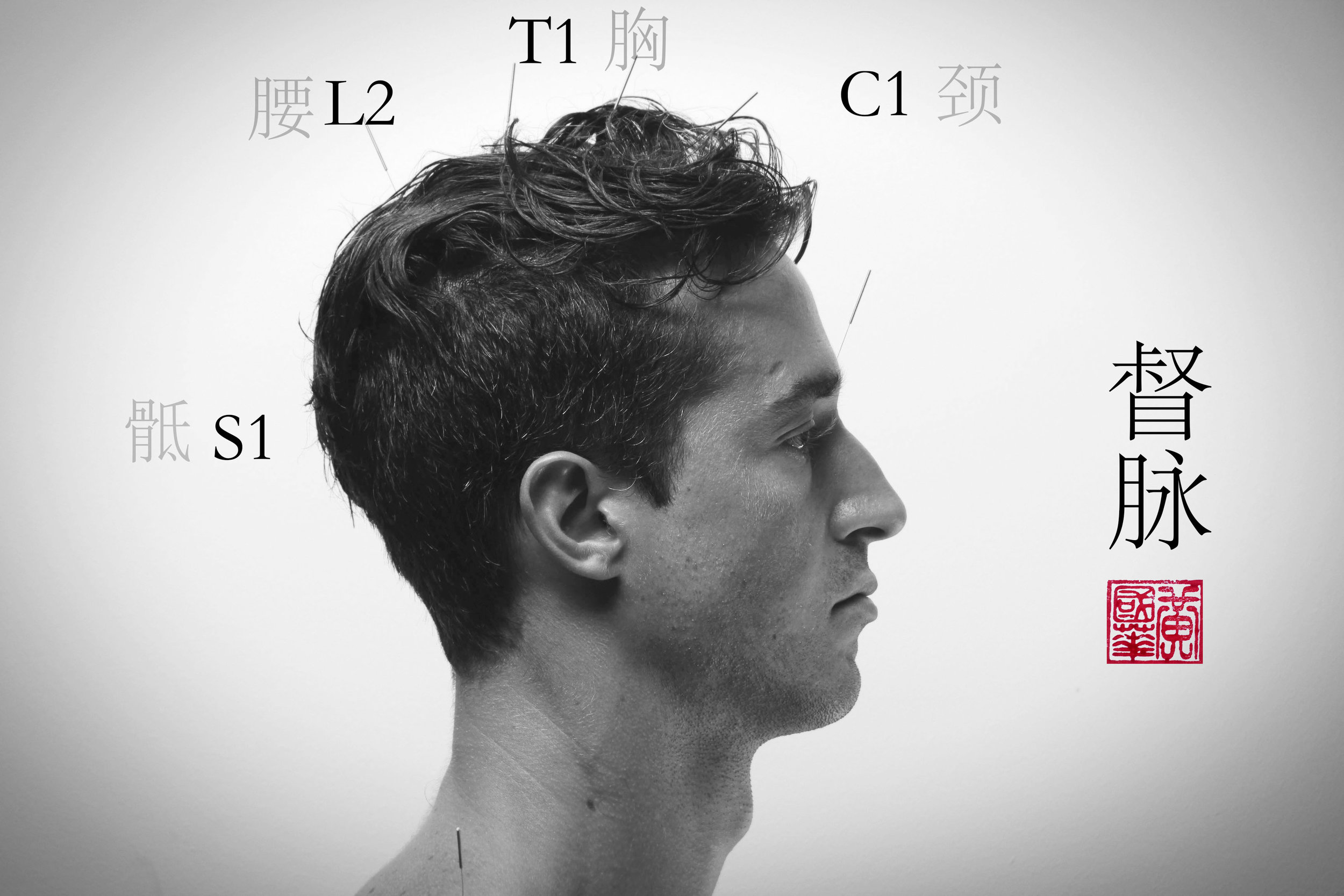
As someone who practices a form of medicine that has a long and illustrious clinical history but a comparatively slimmer amount of randomized research behind it, I tend to be on the receiving end of the blunt instrument of the evidence-based ideal. (Which should be changing, by the way! We now have MRI and other objective measures of outcomes for certain conditions, but not all, though the mechanisms of acupuncture are still not close to settled). Recently, I received a letter from an insurance company in Utah stating that in that state, they do not regard acupuncture as a legitimate treatment for pain (in this case, intractable back pain after back surgery). It reminded me of those stickers you see at gas stations stating that gas fumes are known “in the State of California” to cause cancer. As if some knowledge extends only to the state line. Utah seems to be fairly unique in this regard, luckily, but that makes it all the odder: why, in light of acupuncture’s acceptance by the majority of state boards of worker’s compensation, by many private insurance companies, and by the National Institutes of Health, does Utah conclude that it’s not appropriate? Probably because it presents another avenue to deny payment; this seems to be the rationale for insurance – they are in the business of denying claims, while selling a product that promises to pay for them.
What the State of Utah doesn’t seem to know is that they are already paying a lot of money for other interventions that are known to not work that well, or don’t work any better than much less expensive treatment options. For instance, a study once compared surgery to “nonoperative care” (defined very broadly) for herniated lumbar disks. It turns out that patients improved substantially from both treatments nearly identically. The major difference seems to be the cost: having a disk removed surgically is much more expensive than, say, physical therapy, analgesic medications or home exercise instruction. Another technique, epidural steroid injections, seems to provide much less relief than previously assumed, according to another recent study.
So, acupuncture, which is cheap and safe, is denied even for a brief prospective course, but surgery and steroid injections are routinely paid for, common sense seems to have been abandoned in the name of the “evidence-based.” If expensive and invasive techniques don’t seem to perform better than “unproven” techniques such as, say, acupuncture, this information somehow doesn’t make it into the healthcare equation. In the end, I think it comes down to certain unacknowledged prejudices in the American medical and insurance models: if it’s not potentially deadly or really expensive, then it isn’t medicine. Though it would seem to be to the advantage of the insurance companies to pay for the least expensive, least invasive treatments first, that’s not what happens.
We are quickly reaching the limit of our high-tech, expensive medical model, however, since it is getting to be financially out of reach for many Americans. What will happen when it becomes clear there is not enough money to test every conceivable treatment in a randomized clinical trial? Hopefully, a more pragmatic model of medicine will emerge, based on not only the “gold standard” of double-blind research, but on the humbler ideals of common sense, accessibility and choice.
_
When Medicine Is Not In Evidence • Written by Benjamin Hawes